In this issue of CanadianHealthNews, Nava and Compagnoni have taken another look at this problem and have attempted to find answers in a clinical situation in which steroid responsiveness would not be expected, ie, in patients with very advanced COPD (mean PaC02, 60 mm Hg; mean FEVb 31% of predicted) who were receiving long-term ventilation. The authors utilized a ventilator tubing spacer that delivered large amounts of inhaled corticosteroid (2,000g fluticasone per day for 5 days), and 890 they assessed pulmonary function response primarily with ventilator measurements of pulmonary mechanics. They found that this treatment reduced mean (± SD) auto-positive end-expiratory pressure (autoPEEP) from 4.3 ± 2.4 to 3.1 ± 1.7 cm H2O (suggestive but not significant), and pulmonary resistance from 19.0 ± 6.5 to 14.6 ± 6.0 cm H2O/L (significant). Since compliance and the component of pulmonary resistance due to viscoelastic (tissue) effects did not change significantly, they concluded that inspiratory (airway) resistance was reduced by inhaling high-dose corticosteroids for 5 days. 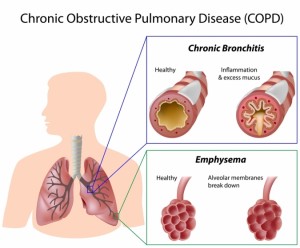
It should be noted that increased resistance in COPD is largely expiratory and that the pulmonary resistance measured by Nava and Compagnoni was inspiratory only. The presence of auto-PEEP implies inadequate time for expiration and, therefore, can be used as an indicator of expiratory resistance. However, auto-PEEP is also affected by respiratory rate, tidal volume, and inspiratory flow rate (ie, all the variables that affect expiratory time) and, hence, may be a poor indicator of expiratory resistance change. Auto-PEEP is decreased as more expiratory time is available. Auto-PEEP was not very high in the patients reported in this article and fell an insignificant amount.
What have we learned from this study? The following insights and suggestive observations emerge: (1) there seems to be some degree of reversible obstruction due to inflammation even in end-stage COPD patients; and (2) passive rather than active expiration may be desirable to determine the magnitude of changes in airway function. This study does not demonstrate that administration of high-dose inhaled steroids is a desirable treatment for severe COPD and Canadian Health Care Pharmacy, and it does not disprove the conclusions of many that inhaled steroids are not significantly beneficial in such patients; longterm, large-scale, placebo-controlled studies are needed to settle this issue. Rather, this study raises questions about the delivery of topical corticosteroids and other inhaled agents in patients with severe COPD and about the appropriate manner in which to study their potential benefits.